|
What does it mean to "die with dignity?"
Five US states allow individuals to choose when to end their lives due to a terminal illness. Many safeguards are in place to guide the process and prescription of the lethal medication. Brittany Maynard is a 29 year old woman with end-stage brain cancer. Her story is all over the internet, and not all information that is posted is accurate. My hope is that her story and advocacy will raise our awareness and start a discussion. There is a lot of controversy over the topic, which is not surprising, it really is a "life or death" topic. Get real information, think about it, and talk with your loved ones. None of us know when a terminal illness or major accident is going to happen. For more information go to: Article about Brittany Maynard Death With Dignity How to Die in Oregon - movie
 Death. Almost no one wants to talk about it, yet we all have to face it some day. The thing to keep in mind is that we each have choices about how we would (ideally) like our death to go. I was listening to NPR the other day, and they had a Radiolab segment on death that got me thinking more about what I want personally, and how important it is to think about (and document!) these things in advance. There was a particularly interesting part of the segment where they were talking to doctors about what their end of life choices would be. You might be surprised. As I've been inspired by this, the next few posts will be about death. I think that contemplating death can very much affect how we live. It's definitely worth giving it the time of day. Contemplatively, Tamara  The holidays mean many different things to different people, but some remain constant. Usually we all see our families at some point, which can be relaxing and stressful, all at the same time. We also end up eating, usually too much, then taking a nap. While these things can be relaxing and a break from the hustle and bustle of the rest of the year, it can also lead to some stressful situations. Here are 5 tips on taking care of yourself during the holidays (or any days). 1. Get enough sleep. Yeah, there are those late nights, staying up playing board games with family, or having long conversations with your cousin that you haven't seen in 2 years. However, as much as possible, maintain your sleep schedule that you have the other 360 days a year. Staying up late and sleeping in can throw off your Circadian Rhythm. There are many benefits to getting enough sleep. If that's not enough, think about how rough it will feel to go back to work on January 2nd, when you've become used to sleeping in until 10am. 2. Eat (as) healthy (as you can). I know, Christmas cookies, your mom's famous cheesecake, etc. etc. I'm not saying don't partake. But just be conscious. Many times, people are conscious of their eating habits all of the other days of the year, but around the holidays, they let anything fly. A little moderation never hurt anyone. I didn't say 3. Breathe. Oh how easy it is to forget to do this basic life-sustaining activity. Yes, our bodies do it automatically, but have you ever noticed that when you're stressed, you hold your breath? To become more conscious of your breath, try "Square Breathing," count while you breathe. Inhale 1-2-3-4, Hold it in 1-2-3-4, Exhale 1-2-3-4, Hold 1-2-34 and repeat. Focusing on your breath not only brings more oxygen to your body, it helps ground you in the here and now moment, rather than focusing on anxiety (toward seeing your baby cousin who cries all the time). 4. Create / maintain your boundaries. We all have that awkward uncle (aunt's husband, not related by blood, obviously) who knows which buttons to push and that annoying topic to bring up. The thing is, that's his stuff, not yours. Have you ever contemplated that he might be saying those things because of the reaction he gets out of you? Stand back and look at the situation. Don't let someone else's junk get tossed in with yours. Chances are, you have enough to carry on your own. 5. Take time for yourself. Let's be honest, we give-give-give, and then give some more, especially during the holidays. There is always one more person to visit with, one more set of cookies to bake. But remember to take time for yourself. That might mean taking a hot bath, getting a massage, or going to brunch with your girlfriends. Whatever this looks like for you, make it a point to do at least one thing that's just for you this holiday season. Your family isn't going anywhere. Happy Holidays! Tamara  Last week I wrote about Hospice care. Today I am going to focus on Palliative Care. WHAT is Palliative Care? Palliative Care is an additional layer of support for individuals facing a serious or chronic illness, such as cancer, Chronic Obstructive Pulmonary Disease (COPD), kidney failure, Alzheimer's, Parkinson's, and many more. Individuals seeking Palliative Care might still be seeking aggressive treatment for the illness. Palliative Care can also be started earlier, and then proceed into Hospice as the illness progresses. WHO provides care? Similar to Hospice, Palliative Care is a team-based approach. Members of the team can include:
WHO pays for Palliative Care? Most insurance plans, including Medicaid and Medicare cover the costs of Palliative Care. WHERE is Palliative Care provided? Similar to Hospice, Palliative Care can be provided in a variety of settings - including the hospital, outpatient settings, at home, in a nursing home, or in a residential hospice. Again, it is not a place where you go, just like Hospice, Palliative Care comes to you. ARE Hospice and Palliative Care the same thing? While some of their components overlap, they are not the same thing. Some of the similarities include: focus on quality of life, a team approach, an added layer of support, family and caregiver care, as well as pain and symptom management. HOW is Hospice different than Palliative Care? Here are a couple of the main differences. Hospice
Example: Betty receives a diagnosis of advanced lung cancer. The prognosis is not great, but they have some options for how to try to cure her. Betty asks for Palliative Care services to help support her and her family, pain management as she goes through treatment, and the other supportive services that Palliative Care provides. Betty is surrounded by not only her trusted physician, but other experts who are familiar with serious illnesses. They are going to try everything to cure the cancer as best they can. While they do this, Betty's Palliative Care team is helping in many ways to improve or maintain her quality of life. Fast forward 1 year. Betty has gone through multiple treatments for her cancer, but it has still advanced. At this point, her primary physician and Palliative Care physician agree, she has less than 6 months left of life. They suggest that she move forward with Hospice care. Betty then gets a new team of support, who are familiar with end of life care. They are focused on making her as comfortable as possible. They also are helping her family cope with the loss they are about to experience. Betty is able to live at her daughter's house because she is familiar with her space and comfortable there. Her Hospice care team takes great care of her, even when she is in her own bed. Her family feels comforted as well, knowing that expert care is only a phone call away, 24/7. Fast forward 4 months. Betty has died. She was surrounded by her children, and her Hospice care team arrive shortly after. Her children are having a hard time dealing with the loss of their mother, so they seek bereavement counseling from the Hospice team for the next 13 months. For more information on Palliative Care, go to the Get Palliative Care website, as well as this particular handout.  November is a month full of awareness and resources for seniors. In addition to Caregivers, and Alzheimers Awarenesses, November is National Hospice and Palliative Care Month. Many people wonder what Hospice actually is, and there are many myths about it. This post will focus on the myths and truths of Hospice, and next week will focus on Palliative care. WHAT is Hospice? Hospice is a special support for individuals and families facing a terminal illness. Hospice is a team-based care model, with a focus on caring, not curing. Individuals on Hospice have a prognosis of 6 months or less to live, verified by 2 physicians. Hospice has been around since 1967, when physician Dame Cicely Saunders opened the first modern hospice in the United Kingdom. WHO provides care? A Hospice team is on-call 24 hours a day, seven days a week. Members of a Hospice team can include:
WHAT kind of care do they provide?
WHO pays for Hospice? Hospice care is covered under Medicare, Medicaid, most private insurance plans, HMOs, and other managed care organizations. Click here for more information on the Medicare Hospice Benefit. WHERE "is" hospice? More often than not, Hospice is not a place where a person goes. Under most circumstances, the Hospice team comes to you. However, there are residential Hospices in the twin cities metro area where your family member can receive care, rather than being at home or in a nursing home. North Memorial Residential Hospice is one example. (I have personally been there and can attest that it is a beautiful, lovely place, with great Hospice care staff.) WHAT HOSPICE IS NOT
For more information on Hospice and Palliative care, go to the National Hospice and Palliative Care Organization and Caring Connections websites. 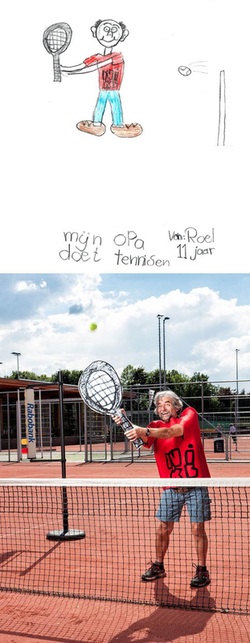 Take a break from your Friday and look at these adorable pictures. A designer in the Netherlands had children draw pictures of their grandparents, and then recreated the drawings in real life. Go here for the full display.  In addition to National Family Caregivers Month, November is of special importance for individuals and families experiencing Alzheimer's Disease. I've found that commonly, the term "Alzheimer's" is misunderstood. I've heard people breaking it down as "Alzheimer's -- Alt, like "Old" in German, as in, Old Timer's".. as if it was a normal part of aging. The thing is, it's not. The name Alzheimer's originated in 1901, when German psychiatrist Alois Alzheimer identified the first case of what came to be known as Alzheimer's Disease. The Alzheimer's Association website provides great information and resources. Below are the basics about Alzheimer's. Click here for the full website. Alzheimer's is a type of dementia that causes problems with memory, thinking and behavior. Symptoms usually develop slowly and get worse over time, becoming severe enough to interfere with daily tasks.
Alzheimer's and dementia basics
 Caregiving can be many things. It can be rewarding, enlightening, and at many times very enjoyable. It can also be exhausting, mentally and physically. November is National Family Caregivers Month. As you reflect on your role as a caregiver, now is a great time to think about ways you can take care of yourself. It is important to give care not only for your family member, but also for you. What are some ways that you can take care of yourself in this next month? Maybe you could..
The important thing is that you make time for yourself. For me, I'm going to go have a cup of tea. Here are some great resources for caregivers. http://caregiveraction.org/ http://www.alz.org/care/honor-caregiver.asp |
Details
AuthorTamara will be posting about topics relevant to caregivers and seniors. More conversations take place on our Facebook Page. Archives
April 2015
Categories
All
|

 RSS Feed
RSS Feed